COMING SOON
Book 2
(Estimated release date - April 2014)
Sign up by email to be the first to get a sneak peek of the cover reveal and release date for book two in the Tempest series.
https://docs.google.com/forms/d/18iyXxpLcjDaUOtH0QCRDCKDLaeZd0smiANfOjfsUVyY/viewform
HEROIN FACTS PROVIDED BY THE NATIONAL INSTITUTE ON DRUG ABUSE
Heroin is an opioid drug that is synthesized from morphine, a naturally occurring substance extracted from the seed pod of the Asian opium poppy plant. Heroin usually appears as a white or brown powder or as a black sticky substance, known as “black tar heroin.”
In 2011, 4.2 million Americans aged 12 or older (or 1.6 percent) had used heroin at least once in their lives. It is estimated that about 23 percent of individuals who use heroin become dependent on it.
HOW IS HEROIN USED?
Heroin can be injected, inhaled by snorting or sniffing, or smoked. All three routes of administration deliver the drug to the brain very rapidly, which contributes to its health risks and to its high risk for addiction, which is a chronic relapsing disease caused by changes in the brain and characterized by uncontrollable drug-seeking no matter the consequences.
HOW DOES HEROIN AFFECT THE BRAIN?
When it enters the brain, heroin is converted back into morphine, which binds to molecules on cells known as opioid receptors. These receptors are located in many areas of the brain (and in the body), especially those involved in the perception of pain and in reward. Opioid receptors are also located in the brain stem, which controls automatic processes critical for life, such as blood pressure, arousal, and respiration. Heroin overdoses frequently involve a suppression of breathing, which can be fatal.
After an intravenous injection of heroin, users report feeling a surge of euphoria (“rush”) accompanied by dry mouth, a warm flushing of the skin, heaviness of the extremities, and clouded mental functioning. Following this initial euphoria, the user goes “on the nod,” an alternately wakeful and drowsy state. Users who do not inject the drug may not experience the initial rush, but other effects are the same.
Regular heroin use changes the functioning of the brain. One result is tolerance, in which more of the drug is needed to achieve the same intensity of effect. Another result is dependence, characterized by the need to continue use of the drug to avoid withdrawal symptoms.
INJECTION DRUG USE AND HIV AND HCV INFECTION
People who inject drugs are at high risk of contracting HIV and hepatitis C (HCV). This is because these diseases are transmitted through contact with blood or other bodily fluids, which can occur when sharing needles or other injection drug use equipment. (HCV is the most common blood-borne infection in the Unites States.) HIV (and less often HCV) can also be contracted during unprotected sex, which drug use makes more likely.
Because of the strong link between drug abuse and the spread of infectious disease, drug abuse treatment can be an effective way to prevent the latter. People in drug abuse treatment, which often includes risk reduction counseling, stop or reduce their drug use and related risk behaviors, including risky injection practices and unsafe sex. (See box, “Treating Heroin Addiction.”)
WHAT ARE THE OTHER HEALTH EFFECTS OF HEROIN?
Heroin abuse is associated with a number of serious health conditions, including fatal overdose, spontaneous abortion, and infectious diseases like hepatitis and HIV (see box, “Injection Drug Use and HIV and HCV Infection”). Chronic users may develop collapsed veins, infection of the heart lining and valves, abscesses, constipation and gastrointestinal cramping, and liver or kidney disease. Pulmonary complications, including various types of pneumonia, may result from the poor health of the user as well as from heroin’s effects on breathing.
In addition to the effects of the drug itself, street heroin often contains toxic contaminants or additives that can clog blood vessels leading to the lungs, liver, kidneys, or brain, causing permanent damage to vital organs.
TREATING HEROIN ADDICTION
A range of treatments including behavioral therapies and medications are effective at helping patients stop using heroin and return to stable and productive lives.
Medications include buprenorphine and methadone, both of which work by binding to the same cell receptors as heroin but more weakly, helping a person wean off the drug and reduce craving; and naltrexone, which blocks opioid receptors and prevents the drug from having an effect (patients sometimes have trouble complying with naltrexone treatment, but a new long-acting version given by injection in a doctor’s office may increase this treatment’s efficacy). Another drug called naloxone is sometimes used as an emergency treatment to counteract the effects of heroin overdose.
For more information, see NIDA’s handbook, Principles of Drug Addiction Treatment.
Chronic use of heroin leads to physical dependence, a state in which the body has adapted to the presence of the drug. If a dependent user reduces or stops use of the drug abruptly, he or she may experience severe symptoms of withdrawal. These symptoms—which can begin as early as a few hours after the last drug administration—can include restlessness, muscle and bone pain, insomnia, diarrhea and vomiting, cold flashes with goose bumps (“cold turkey”), and kicking movements (“kicking the habit”). Users also experience severe craving for the drug during withdrawal, which can precipitate continued abuse and/or relapse.
Besides the risk of spontaneous abortion, heroin abuse during pregnancy (together with related factors like poor nutrition and inadequate prenatal care) is also associated with low birth weight, an important risk factor for later delays in development. Additionally, if the mother is regularly abusing the drug, the infant may be born physically dependent on heroin and could suffer from neonatal abstinence syndrome (NAS), a drug withdrawal syndrome in infants that requires hospitalization. According to a recent study, treating opioid-addicted pregnant mothers with buprenorphine (a medication for opioid dependence) can reduce NAS symptoms in babies and shorten their hospital stays

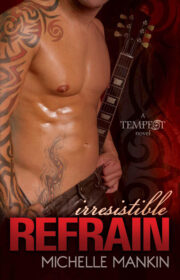
"Irresistible Refrain" отзывы
Отзывы читателей о книге "Irresistible Refrain". Читайте комментарии и мнения людей о произведении.
Понравилась книга? Поделитесь впечатлениями - оставьте Ваш отзыв и расскажите о книге "Irresistible Refrain" друзьям в соцсетях.